Blood test predicts tissue injury in kidney transplant recipients
Researchers at UC San Francisco and Rush University Medical Center, Chicago, may have found a predictor for a disorder affecting kidney transplant recipients that can accelerate organ failure, a discovery that eventually could allow for customized therapies and improved patient selection for transplant.
The study of focal segmental glomerulosclerosis (FSGS), a devastating form of kidney disease, is in the Oct. 1 issue of Science Translational Medicine. Research was conducted by an international study team, with Necker Hospital in Paris and UCSF joint lead authors and Rush University Medical Center and UCSF joint senior authors.
"This is a new blood test to monitor patients before kidney transplant and predict who may have recurrence of FSGS, thereby preventing loss of kidneys," said co-senior author Minnie Sarwal, MD, PhD, professor of transplant surgery at UCSF.
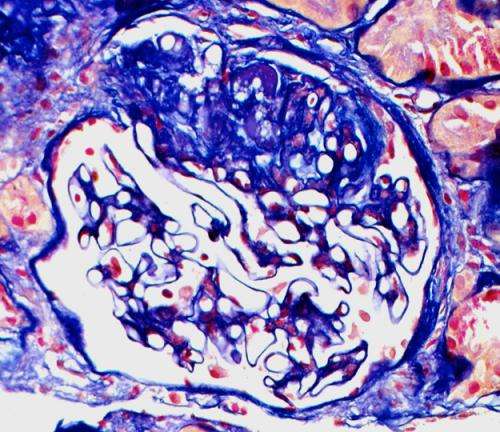
In the kidneys, the glomeruli serve as filters, helping rid the body of unnecessary or harmful substances. After a kidney transplant, scar tissue can form on parts of the donated kidney glomeruli, causing FSGS.
Kidney transplant patients with FSGS face a high risk of disease recurrence, 20-40 percent after a first transplant and up to 80 percent after a second. Its causes are largely unknown and may include circulating proteins and antibodies. Recurrence is managed by immunosuppressive drugs along with current standards of treatment that include salt restriction, diuretics and steroids, plasma filtration, and immunoadsorption.
"The clinical and economic impact of changing the course of FSGS recurrence has far-reaching implications," the study authors wrote. "These include improved graft survival, reduced patient morbidity, reduced cost of salvage therapies including dialysis, and the preservation and increased availability of transplant organs."
In their research, Sarwal and her colleagues used high-density protein tests to process 141 serum samples from 98 patients (64 with FSGS) before and one year after transplant surgery. Patients were from four transplant programs in the United States and Europe.
Of the approximately 9,000 antigens (foreign or toxic substances) screened, the tests identified antibodies against 789 antigens that were significantly increased in patients at risk for FSGS. In further studies using mice, the antibody levels in a protein called CD40 had 78 percent prediction accuracy for FSGS, while a panel of seven out of 10 antibodies that target glomerular antigens increased the accuracy to 92 percent.
As a result, a pre-transplant antibody panel that included anti-CD40 antibodies – named FAST for "FSGS Antibody Screen for Transplant" – could be a good predictor for FSGS. Using FAST, the researchers even learned the antibody signature in FSGS patients remains a year after transplant, despite intensified immunosuppressive therapy and plasma exchange.
"We found that during FSGS recurrence, the antibody binding to the CD40 protein in the podocytes of the kidney drives injury to the kidney's filtering unit with leakage of protein and scar tissue, and blocking this CD40 antibody appears to reverse injury," Sarwal said. "This suggests CD40 blockade in kidney transplant patients may help cure the disease. This drug already is beneficial for organ transplants due to its immunosuppressive properties, so it would be a very attractive new drug for FSGS recurrence prevention in kidney transplants."
Podocytes are cells in the Bowman's capsule of the kidneys that wrap around the glomerulus capillaries. The Bowman's capsule performs the first step in filtering blood to form urine.
Another study highlight is the observation that patient-derived antibodies against CD40 functionally cooperate with a previously identified culprit of FSGS called soluble urokinase plasminogen activator receptor (suPAR). Co-injection of patient-derived CD40 anti-autobodies and suPAR caused enhanced kidney filter failure more than each component did by itself.
"This is an important, novel discovery of a pathogenic antibody synergizing effects with a circulating factor that further sheds light on the enigmatic problem in kidney transplantation, i.e., FSGS recurrence," said study co-senior and co-correspondent author Jochen Reiser, MD, PhD, Ralph C. Brown MD professor and Chairman of Medicine at Rush University Medical Center.
According to Sarwal, additional study of the FAST panel is needed, followed by a clinical trial in collaboration with a pharmaceutical company of an anti-CD40 drug.
"We want to predict FSGS recurrence before we put a kidney in," said Sarwal, who conducted the research while at Stanford University and has since moved her entire lab to UCSF. "We then can treat the high-risk patients with a new drug to possibly prevent disease."
More information: "A circulating antibody panel for pretransplant prediction of FSGS recurrence after kidney transplantation," by M. Delville et al. Science Translational Medicine, 2014. stm.sciencemag.org/lookup/doi/ … scitranslmed.3009278















