Key to blocking influenza virus may lie in a cell's own machinery
Viruses are masters of outsourcing, entrusting their fundamental function - reproduction - to the host cells they infect. But it turns out this highly economical approach also creates vulnerability.
Researchers at Rockefeller University and their collaborators have found an unexpected way the immune system exploits the flu virus' dependence on its host's machinery to create new viruses capable of spreading infection. This discovery suggests a new approach to combating winter's most unpleasant, and sometimes, deadly curse: the seasonal flu.
"Influenza A, the virus we studied, relies on a host's protein-cutting machinery to put the final touches on new viral particles. Our research has shown that the host immune system fights back by turning off this machinery," says study researcher Charles Rice, Maurice R. and Corinne P. Greenberg Professor in Virology Professor and head of the Laboratory of Virology and Infectious Disease. "This concept, that a host would inhibit its own protein-cutting enzymes in order to fight off a virus, is entirely new."
Experiments described today (February 12) in Cell reveal a new function for the well-studied protein known as PAI-1 (plasminogen activator inhibitor 1) as the key to this defensive strategy. PAI-1 shuts down proteases, which are enzymes that break the chemical bonds within protein molecules. PAI-1 is best known for inhibiting proteases involved in the break down of blood clots. After seeing evidence of a new role for PAI-1, the researchers found that human and mouse cells unable to properly produce it appeared more vulnerable to infection by influenza A. In experiments, they used the subtype H1N1, a derivative of the 1918 pandemic flu and a member of a large family of flu viruses that include seasonal flu.
A cell infected by a virus releases chemical signals known as interferons, which turn up the volume on a legion of defensive genes. "The hundreds of host proteins produced by these interferon-stimulated genes are like an army. We know that, together, they can effectively defend against a viral infection, but we don't know how the individual soldiers fight back, particularly those that interfere with later stages of viral replication, when the virus exits the cell and spreads the infection," says first author Meike Dittmann, a postdoc in the lab. Previous work here and elsewhere has explored inhibitors of the early stages of viral replication.
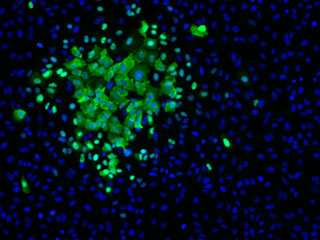
They started out by testing a large suite of genes activated by interferon. With help from Paul Bieniasz's Laboratory of Retrovirology at The Rockefeller University and the Aaron Diamond AIDS Research Center, they introduced these individual genes into cells, then infected the cells with the flu. With the knowledge that influenza A's replication cycle takes about eight hours, they watched to see which genes blocked the ability of influenza to spread. As expected, numerous genes inhibited late stages infection, but one stood out: SERPINE1, the gene that codes for PAI-1.
Given what was already known about PAI-1, Dittmann suspected how it might help cells fight flu.
"A virus attacks a cell using fusion proteins, and if these don't work properly, new virus particles get out of an infected cell just fine, but they cannot spread the infection to other cells. Proteases activate fusion proteins by clipping them, but on its own influenza A doesn't have the gene for the protease it needs. As a result, the virus relies on the host proteases to do the job," Dittmann says.
Subsequent experiments confirmed PAI-1 did indeed prevent the cutting of the fusion protein, known as hemagglutinin, and that high levels of PAI-1 prevented the virus from producing particles capable of spreading the infection. Furthermore, mice that lacked the gene for PAI-1 generally fared worse than their peers when infected with the influenza A virus. Experiments conducted by the team's collaborators at the MRC National Institute for Medical Research in London used infected tissues cultured from mice's tracheae to confirm PAI-1's role in fighting off the infection.
Human cells were the final step. Researchers in Senior Attending Physician and Professor Jean-Laurent Casanova's St. Giles Laboratory of Human Genetics combed through a database containing genetic information on patients who had suffered from severe infectious disease to find those with genetic changes that reduced PAI-1. Biopsies taken from these patients had been used to create cell lines, and when cells derived from patients with mutations in SERPINE1 were infected, they accumulated higher loads of the virus than cells derived from people without mutations in the gene.
"While this study was conducted with Influenza A, our results may have broader implications," Rice says. "PAI-1 is part of a large family of protease inhibitors, and it's possible that it, or its close relatives, may interfere with the replication of other viruses that don't carry genes for their own proteases. This suggests that it may be possible to use a PAI-1-like strategy as a treatment for flu, and possibly other viral infections."




















