New breast cancer screening analysis confirms biennial interval optimal for average risk women
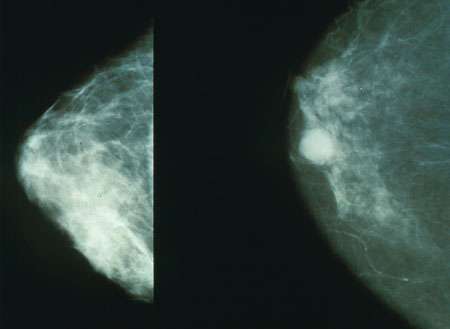
Results from a second comprehensive analysis of mammography screening, this time using data from digital mammography, confirms findings from a 2009 analysis of film mammography: biennial (every two years) screening offers a favorable balance of benefits to harm for women ages 50 to 74 who have an average risk of developing breast cancer.
A technical report of the analysis is posted on the US Preventive Services Task Force's website and is cited as one piece of evidence for its 2015 draft recommendations for breast cancer screening with mammography.
The new results represent a unanimous consensus of six independent modeling research teams from eight academic institutions that are part of CISNET, the NCI-funded Cancer Intervention and Surveillance Modeling Network, as well as researchers from the Breast Cancer Surveillance Consortium (BCSC).
The new CISNET/BCSC study used the six different simulation models to analyze 10 different digital breast cancer screening strategies for the U.S. female population with varying risk levels and competing causes of death other than breast cancer.
"No individual woman should base her decision on when to screen for breast cancer on these model findings," says the paper's lead author, Jeanne S. Mandelblatt, MD, MPH, of Georgetown Lombardi Comprehensive Cancer Center, a CISNET member. "We are modeling the population. The right answer about when to start screening and how often to have mammography will be determined individually, based on a woman's own risk and her preference for going through possible false positive tests. No model can provide answers to that.
"The tradeoff a woman is faced with is that every time she undergoes a screening test, she runs a risk of having a false-positive result that might lead to more testing and biopsies, or perhaps overtreatment," Mandelblatt says. "Overtreatment occurs when a women gets surgery, chemotherapy, and/or radiation for a cancer that is not destined to become life threatening."
The researchers used their models to examine screening strategies with different starting ages (40, 45 or 50), stopping ages, and one- or two-year intervals between screening exams. The modeling uses national data on breast cancer incidence, risks for breast cancer, mammography characteristics, treatment effects, and risk of dying from other diseases and then estimates the lifetime impact (outcomes including benefits and harms) of breast cancer screening mammography across the course of life.
The new analysis also incorporated four molecular subtypes of breast cancer based on hormone receptor and HER2 status, newer treatments, and information from digital screening and breast density. (Studies have suggested that women with dense breasts are more prone to cancer development. Tumors are also harder to find in dense tissue.)
Among the other modeling findings is that:
- In an unscreened population, the models predict a median 12.9% cumulative probability of developing breast cancer from ages 40 to 100. Without screening, the median probability of dying of breast cancer is 2.5%.
- If a particular screening strategy leads to a 30% reduction in breast cancer mortality, then the probability of breast cancer mortality would be reduced from 2.5% to 1.8%—or 7.5 breast cancer deaths averted per 1000 women screened.
- Screening biennially from ages 50-74 achieves a median 25.8% breast cancer mortality reduction—averting 7 breast cancer deaths per 1000 women screened and leads to 953 false positives.
- Biennial strategies maintain an average of 81.2% of annual screening benefits with almost half the false positives and fewer over-diagnosed cases. (Over-diagnosis occurs when the cancer is small and was never destined to become life threatening or because a woman can die of other illnesses before her breast cancer surfaces.)
- Compared with biennial screening from ages 50-74, starting biennial screening at age 40 averts one more death from breast cancer and generates 576 more false positive tests and one more over-diagnosed cancer for every 1000 women screened.
- Annual screening of average risk women would avert 3 more breast cancer deaths, but yields 1988 more false positives and 7 more over-diagnoses per 1000 women screened compared to screening every other year from 50-74.
- For women with a two- to four-fold increase in breast cancer risk in their 40s compared with the average population in their age group, annual screening starting at age 40 or 45 would have a similar or more favorable harm to benefit ratio as biennial screening of average risk women from 50-74.
- For women with even a 1.3-fold increase in risk (the level seen with high breast density or obesity, for example), biennial screening starting at age 40 would have similar ratios of harms to benefits as expected under biennial screening of average risk groups from ages 50-74.
- For healthy older women who have an average of a 17-year remaining life expectancy, screening would be reasonable through age 78 or 80 and would have a minimal increase in over-diagnosis compared with stopping at age 74. However, for women with moderate to severe illnesses, screening cessation could occur at about age 68.















