Body's response to injury and inflammation may hinder wound healing in diabetes
One of the body's own tools for preventing wound infections may actually interfere with wound healing, according to new research from Boston Children's Hospital. In a study published online in Nature Medicine, scientists from the hospital's Program in Cellular and Molecular Medicine (PCMM) found they could speed up wound healing in diabetic mice by keeping immune cells called neutrophils from producing bacteria-trapping neutrophil extracellular traps (NETs).
The study, led by PCMM senior investigator Denisa Wagner, Ph.D., and postdoctoral fellow Siu Ling Wong, Ph.D., suggests that methods of preventing NET production or of cleaving NETs in a wound could, one day, possibly help alleviate wound healing problems in patients with diabetes.
Delayed wound healing is a common complication of both Type 1 and Type 2 diabetes. Open diabetic foot ulcers, for example, affect a quarter of people with diabetes and are a leading cause of amputations.
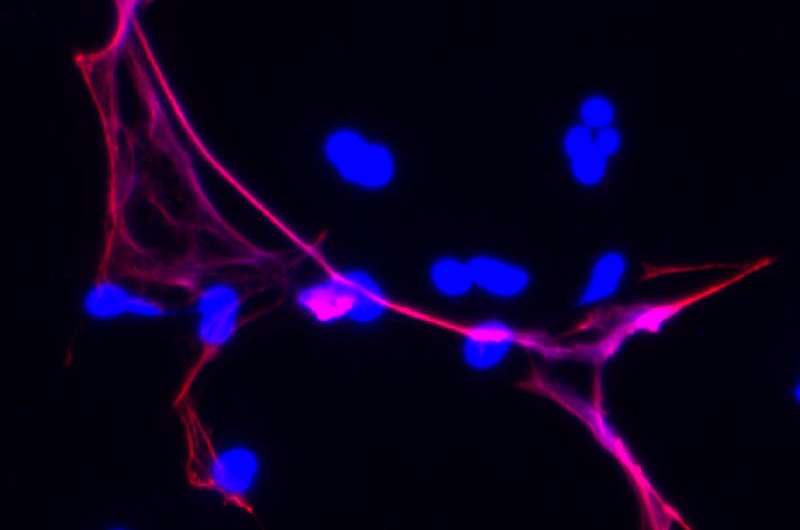
When the skin is cut or broken, the body mobilizes a complicated array of cells and proteins to stop bleeding, prevent infection by triggering inflammation and start the healing process. As part of the inflammatory response, neutrophils, which ingest and destroy bacteria, expel their own chromatin (a mix of DNA and associated proteins) in the form of NETs within the wound.
While possibly beneficial as a tool for keeping bacteria out of the body, NETs also have a dark side. 'NETs predispose patients to inflammation, heart disease and deep vein thrombosis [dangerous blood clots that form within veins deep inside the body], all of which are elevated in patients with diabetes,' says Wagner, who is also the Edwin Cohn Professor of Pediatrics at Harvard Medical School.
To see whether diabetes primes neutrophils to produce NETs, Wagner, Wong and colleagues at Joslin Diabetes Center and Pennsylvania State University examined neutrophils from patients with either Type 1 or Type 2 diabetes, finding that the cells contained four times the normal amount of PAD4 (a key enzyme in the NET production process) and made more NETs when stimulated. Further lab experiments revealed that neutrophils from healthy donors or mice when exposed to excessive glucose—mimicking the diabetic environment—were also more likely to release NETs than those incubated in normal glucose levels.
Diabetic mice in the study had more NETs in wounds and healed more slowly than normal mice. However, Wagner and Wong's team found that healing was accelerated in diabetic mice that lacked PAD4 (and therefore could not produce NETs).
To see whether cleaving NETs would have an effect similar to preventing their production, the research team treated mice with DNase 1 (an enzyme that breaks up DNA and therefore can destroy NETs). After three days, wounds on DNase 1-treated diabetic animals were 20 percent smaller than on untreated animals. Interestingly, DNase 1-treatment appeared to accelerate wound healing in healthy mice as well.
Wagner and Wong explain that NETs may impede wound healing in part because the dense, toxic mesh they produce interferes with new skin cells trying to enter the wound site. They also suggest that NETs may be redundant as a defense mechanism against bacteria.
'We don't fully understand the functions of NETs, but all of the other antimicrobial functions of neutrophils are preserved even if they cannot make NETs,' Wagner notes. 'Any injury that causes inflammation will result in production of NETs, and we think that if the injury involves skin repair, NETs will hinder the repair process.'
More information: Diabetes primes neutrophils to undergo NETosis, which impairs wound healing, Nature Medicine, DOI: 10.1038/nm.3887
















