Putting exercise under the microscope
According to the Centers for Disease Control, newly diagnosed cases of type 2 diabetes have quadrupled since 1980, when 4.5 million cases were diagnosed, to 20.9 million in 2011.
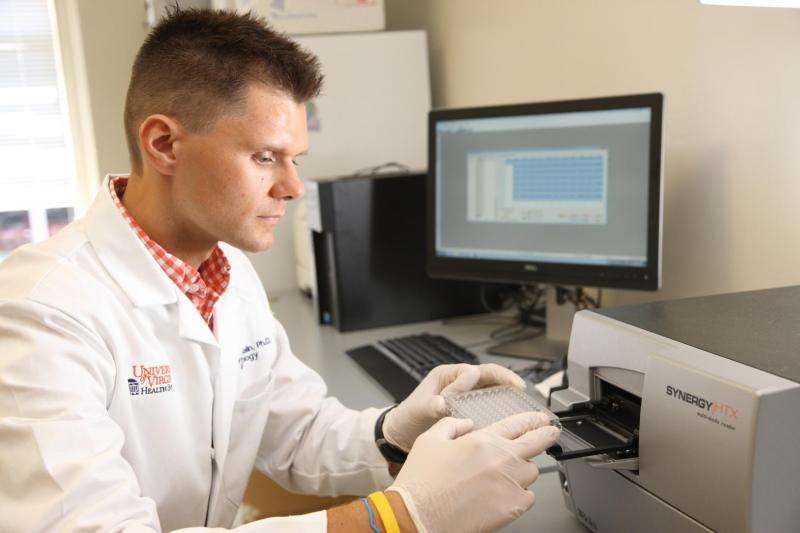
As the nation turns its attention to the prevention and care of diabetes, a new research lab in the University of Virginia Curry's School of Education is looking for ways to slow the rapid increase of new cases.
One project of the Applied Metabolism & Physiology Laboratory, or AMP lab, aims to identify what kind of exercise in what specific intensity most positively impacts individuals diagnosed with pre-diabetes, a precursor to type 2 diabetes diagnosis.
The Curry School's Audrey Breen recently sat down with the lab's director, Steven K. Malin, an assistant professor of kinesiology, to talk about the lab's work.
Q. Why are diabetes diagnoses skyrocketing in America?
A. That's a tricky question to answer. While genetics likely play some role, the rapid rise in diabetes diagnoses over the last 30 years suggests something else must be driving this change.
Leading ideas relate to increased consumption of highly processed foods containing too much sugar or fat as well as an overall lack of time spent exercising. Together these factors likely modify how the body responds to the hormone insulin, which is a very important hormone that controls blood glucose levels. When people eat too much and/or don't exercise enough, insulin does not work as effectively as it should, and often this tips the scales in promoting weight gain and diabetes diagnosis.
At the same time, however, we also have to be aware that stress from work/family, alterations in sleep, and ways in which communities are even being designed today could independently impact our health. So while the cause for diabetes is likely multi-factorial and there is a biological predisposition in some people, it seems clear that lifestyle choices are key driving factors.
Q. What is the goal of the AMP lab's research project focusing on diabetes?
A. We think of exercise as a drug. Just like in pharmacology, you have to take a pill at a given dose, for a specific number of times a day and over a certain period of time in order to get the desired effect. We think of exercise in exactly the same way. A key mission for us is to figure out the optimal exercise dose at which exercise should be prescribed based on the cause of diabetes.
Right now, we are interested in leveraging what we know about interval exercise and testing if interval exercise can significantly impact an individual's blood glucose (sugar) level based on their pre-diabetes status. Interval exercise is a series of exercises that have people exercise at high and low intensity for short periods of time. The patients in our study will participate in both standard of care – or non-interval – exercise and interval exercise.
Our preliminary findings give evidence that when we test the blood sugar of our patients before and after exercise training, the blood sugar is reduced to a greater amount when they engage in interval exercise. We are also trying to understand if the reason for this is due to greater blood flow, increases in pancreatic function or enhanced actions of insulin on skeletal muscle, liver, or adipose tissue metabolism.
Q. You are studying different types of pre-diabetes. How do those types differ from one another and what implications do those differences have on the disease?
A. This is an important question. Diabetes is a complex disease, and it really isn't clear how people develop the disease. There are predominately three different times high blood sugar presents itself: after fasting, such as first thing in the morning; after eating a meal; and both after fasting and after eating. Part of our work is to figure out how the roots of these diseases differ from each other.
In our current study, we are including patients who have high blood sugar after eating and who have high blood sugar after both eating and fasting. The more we can determine how these manifestations of high blood sugar behave differently, originate differently and respond differently to interventions, the better chance we have of effectively treating the disease.
Q. How significant will the impact be on the overall type 2 diabetes diagnosis rate if there are effective ways to treat pre-diabetes?
A. This is potentially huge. Right now we know that accumulating about 150 minutes a week of exercise can delay the onset of type 2 diabetes by about 58 percent when compared to not engaging in healthy lifestyle choices.
While this is very encouraging, it also points to the fact we can do more. If we can optimize our prescription of exercise by targeting the underlying causes, we could significantly decrease the progression rates and/or prevent the development of type 2 diabetes in more people.
Q. The other major projects in the AMP lab focus on obesity and cardiovascular disease. How do these diseases and diabetes relate to each other?
A. Interestingly, the two kinds of pre-diabetes we are studying are known to have high-risk cardiovascular disease. In fact, people with high blood glucose levels after a meal, with or without the high fasting levels, have a one- to two-fold risk of cardiovascular disease compared with healthy counterparts.
Obesity seems to be a central factor in promoting this disease risk. It isn't entirely clear how obesity causes diabetes, but there seems to be good reason to think that obesity causes the action of insulin to be less effective.
To address this issue further, we are also implementing a novel metabolic fitness program for patients undergoing bariatric surgery, a surgical procedure of a patient's digestive system to aid in weight loss. This is critical because many patients undergoing bariatric surgery have pre-diabetes and/or type 2 diabetes and are at high risk for cardiovascular disease. Together, studying these patients in our lab at the same time with different exercise treatments and/or nutrition interventions will allow us to identify optimal ways to lower disease risk and improve overall well-being.
















