Scientists accelerate immune response to tuberculosis in mice
New research findings provide insight into the immune system pathways that may be key to developing an effective tuberculosis (TB) vaccine. The study, to be published Thursday in the journal Nature Communications, was supported by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health.
Globally, an estimated 10.4 million new TB cases occurred in 2015, according to the World Health Organization. A TB vaccine called bacille Calmette-Guérin (BCG) is currently used in countries with a high prevalence of TB to prevent severe forms of the disease in children. However, the protection provided against pulmonary TB in adults is very variable, and people vaccinated with BCG are more likely to give false positives on skin tests for TB.
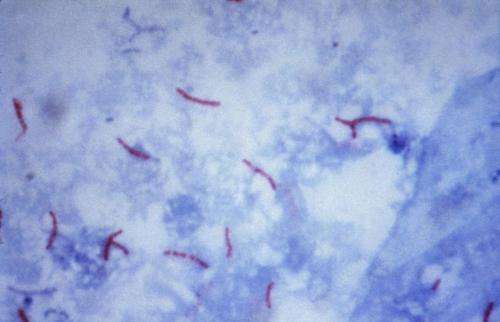
Therefore, researchers are working to create an improved TB vaccine. In animal research, scientists have found that during an infection with the tuberculosis bacterium Mycobacterium tuberculosis, immune system cells called T cells are slow to congregate in the lungs and attack the invaders, allowing for infection to develop despite vaccination.
Previous research has suggested that a key to a faster immune response might lie with dendritic cells that present molecules from bacteria, viruses, and other harmful invaders to disease-fighting T cells, prompting the T cells to attack incoming pathogens. In this new study, scientists led by a group at Washington University in St. Louis investigated whether the delay could be prevented by activating certain immune pathways. First, the researchers established that T cells from vaccinated mice were capable of responding well to TB bacteria. The scientists then introduced dendritic cells that had already been "primed" by exposure to molecules from TB bacteria into the lungs of vaccinated mice, and exposed the mice to different strains of M. tuberculosis. The researchers found that the vaccinated mice that also received activated dendritic cells at the time of infection reached near-sterilizing levels of immunity against TB.
Next, the scientists tried to activate the same immune pathways but without the primed dendritic cells. Specifically, mice vaccinated with the BCG vaccine were treated with two different experimental compounds (amph-CpG and FGK4.5) along with TB antigens designed to activate dendritic cells in the lungs, and then exposed to TB bacteria. The treated mice mounted faster and stronger immune responses against the bacteria, the researchers report.
The scientists note that the technique they used in mice may be impractical in humans because the compounds or activated dendritic cells would need to be applied at the time of infection, which is difficult to predict or detect in the real world. However, the research has led to a better understanding of the mechanisms of TB immunity, which may shape the direction of more effective TB vaccine research in the future, the authors wrote.
More information: K. Griffiths et al. Targeting Dendritic Cells to accelerate T cell activation overcomes a bottleneck in tuberculosis vaccine efficacy. Nature Communications, (2016). DOI: 10.1038/NCOMMS13894




















