New drug provides long-awaited breakthrough for Parkinson's psychosis
Julie Torrence clearly remembers the emotional jolt she felt the day her father, Clyde Hill, failed to recognize her at his Kansas care center.
For nearly three decades, Parkinson's disease had afflicted Hill in a growing number of ways, from the muscle rigidity and walking difficulties that forced his retirement from farming to the more recent hallucinations and delusions that had him trying to break out of the care center. Now he thought his oldest child was his sister.
Torrence cried.
About two months later, she met her father at his doctor's office after he'd spent four weeks on a new drug, the first approved to treat Parkinson's psychosis. Now he knew her name, his doctor's name and the names of his children, grandchildren and great-grandchildren. Even better, he seemed happy again.
In the doctor's office, Torrence cried again.
"You've given us our father back," she told Hill's doctor, Rajesh Pahwa, the director of the Parkinson's Disease and Movement Disorder Center at the University of Kansas Health System.
Most people recognize Parkinson's patients through tremors, slow body movements and other motor problems. Yet up to half of patients develop psychosis at some time during the disease's course, often in the later stages and sometimes as a side effect from drugs prescribed to help motor skills.
Tackling the psychosis has proved difficult, in part because doctors struggled for decades to address the motor problems, Pahwa said. As gains happened there, the nonmotor problems became a bigger and bigger challenge to manage, he said.
Some hallucinations or delusions stay mild or happen infrequently enough that patients can handle them. But others are so scary or difficult to manage that they consume patients and overwhelm their caregivers.
Perhaps a patient has been happily married 50 years but now bitterly believes his or her spouse is having an affair. Or patients may become driven by a fear that strangers or authorities want to hurt them. Some grow so agitated they try to flee their homes or accuse family of colluding with the bad people.
New Yorkers complain of non-existent rats in their apartments. Kansans are more likely to report non-existent cattle in their backyards. One of Pahwa's patients argued with his wife over what he saw in a tree. The patient took a photo to Pahwa to prove that a girl had been sitting there. Pahwa saw only a tree branch.
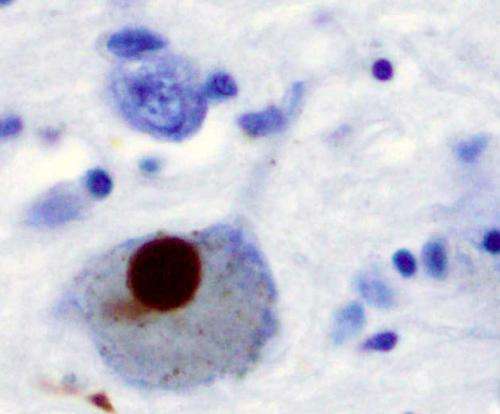
Antipsychotic drugs used for schizophrenia don't help because they block dopamine in the brain, which also is what Parkinson's does as it damages motor functions.
Researchers searched for a chemical compound that could treat psychosis without impairing motor skills. Acadia Pharmaceuticals first synthesized a solution, pimavanserin, in 2001.
It took 15 years to get the product to the market under the brand name Nuplazid, which the Food and Drug Administration approved a year ago this month. Though the drug is expensive, with a one-month wholesale cost of $1,950, insurance often covers most of that. Acadia offers financial assistance for those lacking insurance coverage.
"The biggest thing with the Nuplazid is, it still does not help every patient," said Pahwa, who participated in Nuplazid's clinical studies and serves as a speaker for Acadia.
Because about one in four patients does not improve after taking the drug, research continues on more options. Two other chemical compounds are being developed or tested, Pahwa said.
Of patients who report benefits from Nuplazid, about half experience a dramatic improvement, he said.
That includes the 78-year-old Hill, who lived most of his life on a farm near Weston. His father also suffered from Parkinson's disease.
As a young child, Torrence watched Hill's father - her grandfather - struggle with hallucinations and delusions. He would pick things out of the air, call out names of people not present or grow fearful of something and take off running, even though he normally couldn't run because of the disease. Yet there he was, in his 80s, running from his farm home with a daughter or grandchild giving chase.
Torrence's grandfather didn't live as long with Parkinson's as her father has. Not as many helpful drugs existed then.
Symptoms began hitting Hill at about age 52, when he developed difficulty reaching to get his wallet out of a back pocket. Drugs helped for about a decade, allowing him to keep farming, running his construction business and staying active in the Weston community, where he had served as school board president during Torrence's senior year and built a ball field for the high school.
By his early 60s, with his mobility limited and falls increasing, he had to sell the construction business, retire from farming and give up driving. Deep brain stimulation surgery gave his body a reprieve for several years, but the disease kept progressing until he turned to a wheelchair to get around.
One evening about two years ago, he looked across the floor in his house and asked, "Do you see that puppy jumping in and out of the box?" Torrence told him no and explained that his Parkinson's might be causing him to see the puppy. Next, he saw a non-existent horse on the lawn.
"It got to the point he thought the CIA or bad guys were in the house," Torrence recalled. "He had to get out of there."
Last fall, Hall began getting out of bed two to three times a night, dressing and trying to leave. "It's not safe here," he would say. If one of his children tried to talk him out of leaving, he'd accuse the child of colluding with the bad guys.
The situation forced his children to tearfully search out a care center.
One night last fall, staff at Twin Oaks Health & Rehab in Lansing, Kan., found Hill trying to ram his wheelchair through the glass entry doors because he thought he needed to escape drug dealers. Two of Torrence's brothers got there before Torrence, who lives farther away. Dad insisted to his boys that he had to feed the cows and move the bulldozer. They calmed him by promising to handle the chores.
Not long after that, Hall stopped recognizing some people and remembering the names of others. He also grew combative with the nurses. Torrence called Pahwa seeking help. The doctor already had prescribed Nuplazid to about 25 patients. He talked it over with Hill and explained it might not work. Hill agreed to try it.
After Hill spent four weeks on the new drug, his turnaround stunned Torrence. Her father noticed the difference, too. One recent day, he volunteered to a care center visitor, "I'm on a new drug."
Hill still experiences some mild delusions, Torrence said. His legs have swollen - a side effect some patients develop - but Torrence considers that much better than the psychosis problems.
"It's a miracle drug, as far as I am concerned," she said.
More research is needed to find ways to help more patients, Pahwa said.
"This is still a pretty unmet need," he said. "One drug doesn't help everyone."
©2017 The Kansas City Star (Kansas City, Mo.)
Distributed by Tribune Content Agency, LLC.














