Cellular network identified that 'short circuits' the antitumor effect of immunotherapies
Researchers from The Wistar Institute discovered a novel form of crosstalk among tumor cells and other cell types in the tumor microenvironment, elucidating the mechanism of action of an immunotherapeutic strategy that inhibits tumor-associated macrophages (TAMs) and instructing a more effective use of this therapeutic approach. This work was published online in Cancer Cell.
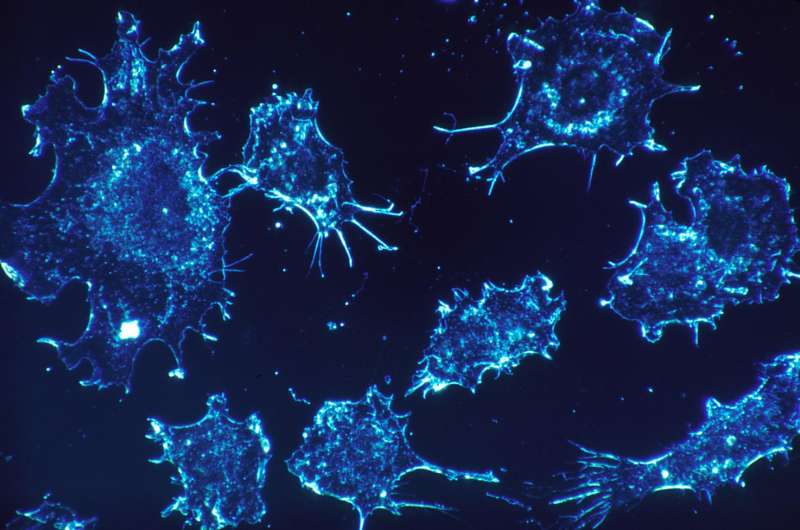
TAMs make up a prominent immune cell population present in the tumor microenvironment. Because of their ability to promote tumor cell proliferation and invasion and inhibit antitumor immune response mediated by T cells, TAMs are considered a potential therapeutic target. Inhibition of the CSF-1 receptor (CSF-1R), which mediates the functions and survival of TAMs, has received interest as a potential strategy to eliminate these cells. However, despite being effective at depleting the TAMs in various tumor models, this strategy has failed to achieve the expected antitumor effects.
"Our findings revealed new aspects of the intricate cellular network that involves tumor cells, TAMs and cancer associated fibroblasts that talk to each other via production of chemical messengers," said Dmitry I. Gabrilovich, M.D., Ph.D., Christopher M. Davis Professor and program leader of the Immunology, Microenvironment and Metastasis Program at Wistar. "We discovered an additional effect of CSF-1R inhibition that brings into play other immunosuppressive cells that sustain tumor progression."
Gabrilovich and colleagues found that, besides depleting TAMs from the tumor site, CSF-1R inhibition also resulted in the unexpected recruitment of polymorphonuclear myeloid-derived suppressor cells (PMN-MDSCs), which favor tumor progression and mediate resistance to immunotherapy approaches. The presence of these cells may explain the lack of antitumor effect by CSF1R inhibition.
The researchers investigated the mechanism of PMN-MDSC recruitment to the tumor site and uncovered an intricate crosstalk that resulted in increased production of signaling proteins responsible for attracting PMN-MDSCs in response to CSF-1R inhibition. In particular, they observed higher levels of Cxcl-1, in this context produced by cancer-associated fibroblasts.
"In order to achieve a therapeutic effect, we realized that we needed to reduce the presence of both immunosuppressive populations, TAM and PMN-MDSC," added Gabrilovich.
By combining the CSF-1R inhibitor with a selective inhibitor of CXCR2, which is the receptor for Cxcl-1 and other molecules whose levels are increased as a consequence of CSF-1R inhibition, they observed significant reduction in tumor growth. In addition, the combination of the two inhibitors together with an immune checkpoint inhibitor resulted in a dramatic antitumor effect, providing additional therapeutic benefits.

















