Scientist finds clearer obesity, diabetes connection

(Medical Xpress)—New findings about the biological links between obesity and insulin resistance and Type 2 diabetes may also shed light on the connection between obesity and cancer, says a scientist at The University of Texas at Dallas.
In a study published in the journal Cell, UT Dallas' Dr. Jung-whan Kim and colleagues at the University of California, San Diego found that a protein called HIF-1 alpha plays a key role in the development of insulin resistance and Type 2 diabetes in obese mice.
The researchers genetically engineered the mice to lack the HIF-1 alpha protein within the animals' fat cells, or adipocytes. The mice still made HIF-1 alpha in other types of cells and tissues in their bodies. Although the mice became obese when fed a high-fat diet, they did not develop insulin resistance and diabetes to near the extent that other obese mice did.
"There is clearly a greater chance among the obese human population to develop insulin resistance and diabetes. We still don't know the exact mechanism, but now we know that HIF-1 alpha is very active in the pathogenesis of these diseases from obesity," said Kim, a co-lead author of the study who conducted the research as a postdoctoral researcher at UC San Diego and the Salk Institute for Biological Studies. He joined the UT Dallas faculty as an assistant professor of molecular and cell biology in 2013.
Kim said the findings about HIF-1—hypoxia inducible factor-1—are significant for their possible application to fighting insulin resistance and diabetes as well as cancer. Here's why:
Cells in the body normally consume oxygen to produce energy. But if oxygen levels decrease—for example, during strenuous exercise or at high altitudes—cells enter a condition called hypoxia, or low oxygen. With oxygen in short supply, cells switch their metabolism. Instead of energy, the cells produce reactive oxygen species, which are molecules that can damage or kill cells. To help mitigate the damage, hypoxic cells activate HIF-1 alpha, which shuts down the production of reactive oxygen species and signals inflammatory cells to migrate to the hypoxic areas.
"Organisms need to be able to temporarily adapt to the stress of hypoxic conditions until the situation changes, so when inflammatory cells see this kind of signal, they come to the hypoxic area to do their normal job, which is to basically eat damaged cells," Kim said.
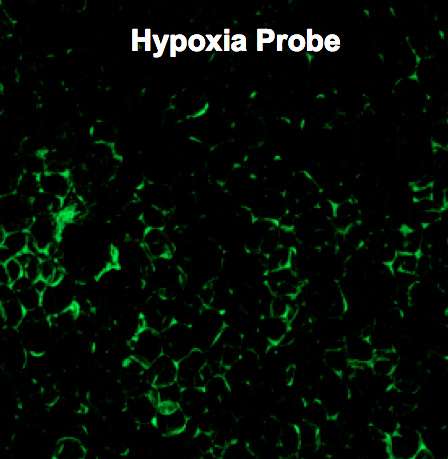
In obesity, however, fat cells are in a chronic state of hypoxia.
"If you look at adipose, or fat tissue, in the obese, there is massive and chronic inflammation," he said. "It's a defense mechanism. The inflammatory cells are really good guys, but as obesity persists, inflammation becomes chronic.
"HIF-1 alpha is important for hypoxia adaptation, but it's constantly activated in the obese, and that's where it turns bad," Kim said. "In the obese, HIF-1 is aberrantly and chronically elevated and is the master regulator of ominous chronic inflammation."
To study the effect HIF-1 alpha might have on the development of insulin resistance and diabetes, Kim and his colleagues used genetic engineering techniques to completely remove, or "knock out," HIF-1 alpha from adipose tissue in obese mice.
"Once we knocked out HIF-1, everything got better," he said. "The fat cells survived and the mice remained obese, but we saw less inflammation in the fat tissue. These mice responded better to insulin than their normal counterparts, which means insulin sensitivity was improved and glucose tolerance was improved."
Kim said several pharmaceutical companies are developing HIF-1 alpha inhibitors, which might one day result in medications to treat Type 2 diabetes and insulin resistance in obese people. But the primary reason behind the push for HIF-1 alpha inhibitors is cancer.
"Tumor cells grow really fast, but the blood vessels that feed them oxygen cannot grow fast enough, so tumor cells become hypoxic," Kim said. "The tumor cells have to develop some sort of mechanism to survive under hypoxic stress, and that's HIF-1 alpha.
"If you can inhibit HIF-1 alpha in a tumor cell, you can kill the cell, and that's why pharmaceutical companies are interested in HIF-1 inhibitors."
Kim said one reason for the study was to gain a better understanding of the links between obesity and cancer.
"There is a clear correlation between the two, but it's not clear why obese people have a greater chance of developing certain cancers," he said. "If you look at breast cancer, the glands that produce milk are completely surrounded by fat cells.
"Tumor tissue is hypoxic. Obese tissue is hypoxic. HIF-1 alpha is important in both conditions. I'm very motivated to study the interaction between breast cancer cells and fat cells."
Lab to Study Fibrosis Role
Dr. Jung-whan Kim's recent study of the relationship between obesity and Type 2 diabetes and insulin resistance has helped spur new research in his laboratory.
Kim has received an I.M. Rosenzweig Junior Investigator Award from the Pulmonary Fibrosis Foundation to support a study into the role the HIF-1 alpha protein plays in fibrosis, which also can occur in the chronically obese. The grant provides $50,000 over two years.
The HIF-1 protein is activated in the body when cells' oxygen levels decrease.
"The presence of HIF-1 alpha results in inflammation," he said. "When the body senses inflammation, it tries to confine that inflammation by secreting collagen. But if the inflammation is chronic, as in obesity, then the process is always activated. The tissue or organ develops excessive fibrous tissue, or fibroids, from this collagen, and then loses function."
One of the more dramatic examples of this condition is pulmonary fibrosis, which develops in the lungs. It's a condition seen in many smokers.
"When you smoke, your lungs experience constant, repeated injury and inflammation, and they develop fibrosis," Kim said. "Healthy lungs are very elastic, but if you have fibrosis, they become stiff and cannot expand.
"We see fibrosis also in adipose tissue, so we are pursuing this research to better understand HIF-1's role in fibrosis in general."















